Reducing Postpartum Haemorrhage in a Nigeria Hospital
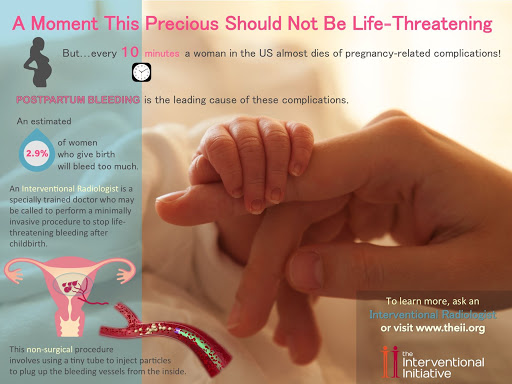 Image credit: the Interventional Initiative
Image credit: the Interventional Initiative
Abstract
Worldwide, over 300 000 women die due to complications of pregnancy and childbirth with most of the deaths occurring in sub-Saharan Africa and India. Postpartum haemorrhage (PPH) accounts for majority of these deaths. For every woman who dies of pregnancy-related causes, 20 to 30 others experience acute or chronic morbidity. PPH is largely due to poor uterine contraction in the third phase of labour, as well as bleeding from peri-partum injuries (episiotomy and perineal tear). Despite the rich evidence of the benefits of appropriate management in reducing PPH, many women do not receive this management due to poor adherence to standards. Review of data over a 16-month period from a private hospital located in the centre of Ilorin, the capital of Kwara State showed that incidence rate for PPH was 8.5%. This is above the average standard in literature (0.9% - 6%). A team set to reduce by half the incidence of primary postpartum haemorrhage rate in the facility within 12 months. The Model for Improvement (MFI) was used for this project. A multi-disciplinary team consisting of doctors, nurses, and management staff used QI tools including Flow Charts, Cause and Effect Diagrams and Pareto charts to identify the root causes and prioritize interventions. Interventions were implemented in 3 cycles of Plan-Do-Study-Act (PDSA). The primary outcome measurement was the monthly PPH rate in the facility. Secondary outcome measurements included rate of episiotomy and perineal tear. Results were monitored over a period of 12 months and the outcomes plotted on a run chart. Following interventions, the monthly incidence of PPH decreased steadily decreased from an average of 8.5% to 4.1%. The episiotomy rate also decreased from 17.1% to 8.5%.